We publish policy-releveant research in high-quality journals
Featured publication
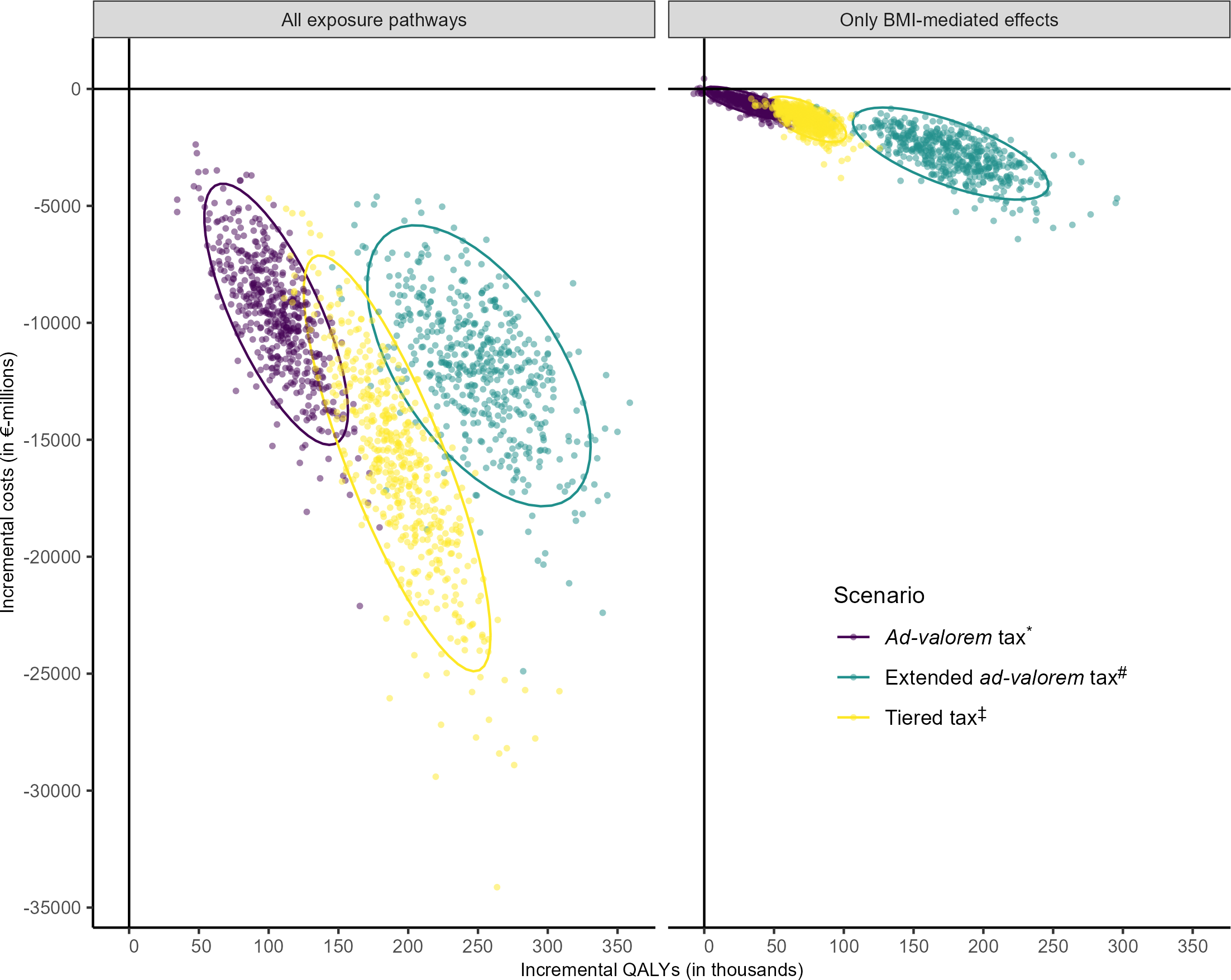
Projected health and economic impacts of sugar-sweetened beverage taxation in Germany: A cross-validation modelling study
PLOS Medicine
21.11.2023
All modelled sugar-sweetened beverages (SSB) taxation scenarios are likely to improve population health and reduce societal costs in Germany by preventing cardiometabolic disease.
Considering all sources of uncertainty, we find that modelled SSB taxation scenarios that lead to reformulation towards less sugar might have a larger population-level health and economic impact than those that incentivize consumer behaviour change only through increased prices.
From a public health perspective, taxation of SSBs should be considered as a policy option for German decision-makers to reduce consumption of added sugar and improve population health.
Highlight figure
Involved researchers
Michael Laxy
Publications showcasing our research
The list below includes a selection of publications by M-CHEP members ordered according to main research areas of the center. Full publication lists can be accessed via the homepages of our members.
Design of health care systems
Kuhn, M., & Nuscheler, R. (2020). Saving the public from the private? Incentives and outcomes in dual practice. Journal of Public Economic Theory, 22(4), 1120-1150. doi: 10.1111/jpet.12447.
Binder, S., & Nuscheler, R. (2017). Risk-Taking in Vaccination, Surgery, and Gambling Environments - Evidence from a Framed Laboratory Experiment. Health Economics, 26(3), 76-96. doi: 10.1002/hec.3620.
Nuscheler, R., & Roeder, K. (2016). To Vaccinate or to Procrastinate? That is the Prevention Question. Health Economics, 25(12), 1560-1581. doi: 10.1002/hec.3268.
Nuscheler, R. & Roeder, K. (2015). Financing and funding health care: Optimal policy and political implementability. Journal of Health Economics, 42, 197-208. doi: 10.1016/j.jhealeco.2015.04.003.
Grunow, M. & Nuscheler, R. (2014). Public and Private Health Insurance in Germany: The Ignored Risk Selection Problem. Health Economics, 23(6), 670-687. doi: 10.1002/hec.2942.
Sundmacher, L., Schang, L., Schüttig, W., Flemming, R., Frank-Tewaag, J., Geiger, I., Franke, S., Wende, D., Weinhold, I., Höser, C., Kistemann, T., Kemen, J., van den Berg, N., Hoffmann, W., Kleinke, F., Becker, U. & Brechtel, T. (2018). Beschluss des Gemeinsamen Bundesausschusses zur Abnahme des Endberichts „Gutachten zur Weiterentwicklung der Bedarfsplanung i.S.d. §§ 99 ff. SGB V zur Sicherung der vertragsärztlichen Versorgung“. Gemeinsamer Bundesausschuss. PDF.
Heiss, F., McFadden, D., Winter, J., Wuppermann, A. & Zhou, B. (2021). Inattention and Switching Costs as Sources of Inertia in Medicare Part D. American Economic Review, 111 (9): 2737–81. doi: 10.1257/aer.20170471.
Farbmacher, H., Ihle, P., Schubert, I., Winter, J. & Wuppermann, A. (2017). Heterogeneous Effects of a Nonlinear Price Schedule for Outpatient Care. Health Econ, 26(10):1234-1248. doi: 10.1002/hec.3395.
Farbmacher, H. & Winter, J. (2013). Per-period co-payments and the demand for health care: evidence from survey and claims data. Health Econ.;22(9):1111-23. doi: 10.1002/hec.2955.
Bünnings, C., Schmitz, H., Tauchmann, H., & Ziebarth, N.R. (2019). The Role of Prices Relative to Supplemental Benefits and Service Quality in Health Plan Choice. Journal of Risk and Insurance, 86(2), 415-449. doi 10.1111/jori.12219.
Valder, F. Reif, S., Tauchmann, H (2024). Diagnosis Related Payment for Inpatient Mental Health Care: Hospital Selection and Effects on Length of Stay. Health Econ. 2024 Dec 8. doi: 110.1002/hec.4920.
Reif, S., & Schubert, S. (2024). Hospital capacity reporting in Germany during COVID-19. Journal of Economic Behavior & Organization, 228, 106730. doi: 10.1016/j.jebo.2024.106730.
Brönneke, J. B., Herr, A., Reif, S., & Stern, A. D. (2023). Dynamic HTA for digital health solutions: opportunities and challenges for patient-centered evaluation. International Journal of Technology Assessment in Health Care, 1-21. doi: 10.1017/S0266462323002726.
Reif, S., Wichert, S., & Wuppermann, A. (2018). Is it good to be too light? Birth weight thresholds in hospital reimbursement systems. Journal of Health Economics, 59, 1-25. doi: 10.1016/j.jhealeco.2018.01.007.
Health services research
Coors, M., Schüttig, W., Reber, K.C., Darius, H., Holzgreve, A., Karmann, S., Stürtz, A., Zöller, R., Kropp, S., Riesner, P., Sundmacher, L. (2024).Cost-effectiveness and cost-utility analysis of a nurse-led, transitional care model to improve care coordination for patients with cardiovascular diseases: results from the “Cardiolotse” study. Eur J Health Econ. doi: 10.1007/s10198-024-01734-7.
Schüttig, W., Darius, H., Reber, K., Coors, M., Flothow, A., Holzgreve, A., Karmann, S., Stürtz, A., Zöller, R., Kropp, S., Riesner, P., Sundmacher, L. (2024). Reducing rehospitalization in cardiac patients: a randomized, controlled trial of a cardiac care management program (“Cardiolotse”) in Germany. BMC Medicine 22, Article number: 480. doi: 10.1186/s12916-024-03691-7.
Iashchenko, I., Flemming, R., Franke, S., & Sundmacher, L. (2023). Do physician networks with standardized audit and feedback deliver better quality care for older patients compared to regular care?: a quasi-experimental study using claims data from Bavaria, Germany. European Journal of Public Health, 33(6), 981–986. doi: 10.1093/eurpub/ckad135.
Geiger, I., Flemming, R., Schüttig, W. & Sundmacher, L. (2023). Regional variations in multimorbidity burden among office-based physicians in Germany. European Journal of Public Health, 33(3), 389-395. doi: 10.1093/eurpub/ckad039.
Flemming, R., Frölich, F., Donner-Banzhoff, N. & Sundmacher, L. (2023). Diffusion of a new drug among ambulatory physicians—The impact of patient pathways. Health Economics, 32(4), 970-982. doi: 10.1002/hec.4650.
Novelli, A., Frank-Tewaag, J., Bleek, J., Günster, C., Schneider, U., Marschall, U., Schlößler, K., Donner-Banzhoff, N. & Sundmacher, L. (2022). Identifying and Investigating Ambulatory Care Sequences Before Invasive Coronary Angiography. Med Care, 60(8), 602–609. doi: 110.1097/MLR.0000000000001738.
Sundmacher, L., Fischbach, D., Schuettig, W., Naumann, C., Augustin, U. & Faisst, C. (2015). Which hospitalisations are ambulatory care-sensitive, to what degree, and how could the rates be reduced? Results of a group consensus study in Germany. Health Policy, 119(11), 1415-1423. doi: 10.1016/j.healthpol.2015.08.007.
Laxy, M., Wilson, E., Boothby, C. & Griffin, S. (2017). Incremental Costs and Cost Effectiveness of Intensive Treatment in Individuals with Type 2 Diabetes Detected by Screening in the ADDITION-UK Trial: An Update with Empirical Trial–Based Cost Data. Value Health, 20(10), 1288-1298. doi: 10.1016/j.jval.2017.05.018.
Laxy, M., Zhang, P., Benoit, S., Imperatore, G., Cheng, Y., Gregg, E., Yang, S. & Shao, H. (2021). Trends in Total and Out-of-pocket Payments for Insulin Among Privately Insured U.S. Adults With Diabetes From 2005 to 2018. Diabetes Care, 44(10), 180–182. doi: 10.2337/dc20-2529.
Wendl, J., Simon, A., Kistler, M., Hapfelmeier, J., Schneider, A., & Hapfelmeier, A. (2022). Identification of target groups and individuals for adherence interventions using tree-based prediction models. Front Pharmacol. doi: 10.3389/fphar.2022.1001038.
Wendl, J., Simon, A., Kistler, M., Hapfelmeier, J., Schneider, A. & Hapfelmeier, A. (2023). Medication Adherence and Healthcare Costs in Chronically Ill Patients Using German Claims Data. Appl Health Econ Health Policy, 21(3), 477–487. doi: 10.1007/s40258-023-00797-6.
Kesternich, I., Caro, F.G., Gottlieb, A.S., Hoffmann, S. & Winter, J.K. (2016). The Role of Outcome Forecasts in Patients' Treatment Decisions--Evidence from a Survey Experiment on Knee Replacement Surgery. Health Serv Res. 51(1):302-13. doi: 10.1111/1475-6773.12311.
Farbmacher, H., Löw, L., & Spindler, M. (2022). An explainable attention network for fraud detection in claims management. Journal of Econometrics, 228(2), 244-258. doi: 10.1016/j.jeconom.2020.05.021
Farbmacher H. (2013). Extensions of hurdle models for overdispersed count data. Health Econ. 22(11):1398-404. doi: 10.1002/hec.2892.
Hafner, L., Biermann, V., Donnachie, E., Hueber, S., Kühlein, T., Tauchmann, H., & Tomandl, J. (2022). Short and medium-term cost effects of non-indicated thyroid diagnostics: Empirical evidence from German claims data. European Journal of Health Economics, 23, doi: 10.1007/s10198-021-01382-1 565-595.
Economics of population health
Emmert-Fees, K., Amies-Cull, B., Wawro, N., Linseisen, J., Staudigel, M., Peters, A., Cobiac, L., O'Flaherty, M., Scarborough, P., Kypridemos, C. & Laxy, M. (2023). Projected health and economic impacts of sugar-sweetened beverage taxation in Germany: A cross-validation modelling study. PLoS Med, 20(11). doi: 10.1371/journal.pmed.1004311.
Pedron, S., Hanselmann, M., Burns, J., Rich, A., Peters, A., Heier, M., Schwettmann, L., Bor, J., Bärnighausen, T., & Laxy, M. (2022). The effect of population-based blood pressure screening on long-term cardiometabolic morbidity and mortality in Germany: A regression discontinuity analysis. PLoS Medicine. doi: 10.1371/journal.pmed.1004151.
Pedron, S., Kurz, C., Schwettmann, L. & Laxy, M. (2021). The Effect of BMI and Type 2 Diabetes on Socioeconomic Status: A Two-Sample Multivariable Mendelian Randomization Study. Diabetes Care, 44(3), 850–852. doi: 10.2337/dc20-1721.
Laxy, M., Zhang, P., Ng, B., Shao, H., Ali, M., Albright, A. & Gregg, E. (2020). Implementing Lifestyle Change Interventions to Prevent Type 2 Diabetes in US Medicaid Programs: Cost Effectiveness, and Cost, Health, and Health Equity Impact. Appl Health Econ Health Policy, 18(5), 713–726. doi: 10.1007/s40258-020-00565-w.
Fan, M., Stephan, A., Emmert-Fees, K, Peters, A. & Laxy, M. (2023). Health and economic impact of improved glucose, blood pressure and lipid control among German adults with type 2 diabetes: a modelling study. Diabetologia, 66(9), 1693–1704. doi: 10.1007/s00125-023-05950-3.
Hapfelmeier, A., Gasperi, C., Donnachie, E. & Hemmer, B. (2019). A large case-control study on vaccination as risk factor for multiple sclerosis. Neurology, 93(9). doi: 10.1212/WNL.0000000000008012.
Gasperi, C., Hapfelmeier, A., Daltrozzo, T., Schneider, A., Donnachie, E. & Hemmer, B. (2021). Systematic Assessment of Medical Diagnoses Preceding the First Diagnosis of Multiple Sclerosis. Neurology, 96(24). doi: 10.1212/WNL.0000000000012074.
Darvishi, S., Donnachie, E., Gasperi, C., Hapfelmeier, A. & Hemmer, B. (2023). Vaccination frequency in people newly diagnosed with multiple sclerosis. Mult Scler, 29(14), 1831–1840. doi: 10.1177/13524585231199084.
Greißel, A., Schneider, A., Donnachie, E., Gerlach, R., Tauscher, M. & Hapfelmeier, A. (2024). Impact of pre-existing mental health diagnoses on development of post-COVID and related symptoms: a claims data-based cohort study. Scientific reports, 14(1). doi: 10.1038/s41598-024-52656-6.
Kesternich, I., Siflinger, B., Smith, J.P. & Winter, J.K. (2015). Individual Behaviour as a Pathway Between Early-Life Shocks and Adult Health: Evidence from Hunger Episodes in Post-War Germany, The Economic Journal, Volume 125, Issue 588, Pages F372–F393, https://doi.org/10.1111/ecoj.12281
Dorn, F., Lange, B., Braml, M., Gstrein, D., Nyirenda, J.L.Z., Vanella, P., Winter, J., Fuest, C. & Krause, G. (2023). The challenge of estimating the direct and indirect effects of COVID-19 interventions - Toward an integrated economic and epidemiological approach. Econ Hum Biol.; 49:101198. doi: 10.1016/j.ehb.2022.101198.
Schwandt, H., Currie, J., Bär, M., Banks, J., Bertoli, P., Bütikofer, A., Cattan, S., Chao, B.Z., Costa, C., González, L., Grembi, V., Huttunen, K., Karadakic, R., Kraftman, L., Krutikova, S., Lombardi, S., Redler, P., Riumallo-Herl, C., Rodríguez-González, A., Salvanes, K.G., Santana, P., Thuilliez, J., van Doorslaer, E., Van Ourti, T., Winter, J.K., Wouterse, B. & Wuppermann, A. (2021). Inequality in mortality between Black and White Americans by age, place, and cause and in comparison to Europe, 1990 to 2018. Proc Natl Acad Sci U S A. 5;118(40):e2104684118. doi: 10.1073/pnas.2104684118.
Bucher-Koenen, T., Farbmacher, H., Guber, R. & Vikström, J. (2020). Double Trouble: The Burden of Child-rearing and Working on Maternal Mortality. Demography; 57(2):559-576. doi: 10.1007/s13524-020-00868-6.
Davies, N.M., von Hinke Kessler Scholder, S., Farbmacher, H., Burgess, S., Windmeijer, F. & Smith, G.D. (2015). The many weak instruments problem and Mendelian randomization. Stat Med. 10;34(3):454-68. doi: 10.1002/sim.6358.
Binder, S. & Nuscheler, R. (2017). Risk-Taking in Vaccination, Surgery, and Gambling Environments - Evidence from a Framed Laboratory Experiment, Health Economics 26(S3), 76-96. doi: 10.1002/hec.3620.
Bünnings C, Hafner L, Reif S, Tauchmann H (2021). In sickness and in health? Health shocks and relationship breakdown: Empirical evidence from Germany, Journal of Economic Behavior & Organization. 190:164-190. doi: 10.1016/j.jebo.2021.07.029
Hafner L, Tauchmann H, Wübker A (2021). Does moderate weight loss affect subjective health perception in obese individuals? Evidence from field experimental data, Empirical Economics. 21 (2021), 2293-2333. doi: 10.1007/s00181-020-01971-8
Global health economics
Reuter, A., Ali, M. K., Mohan, V., Chwastiak, L., Singh, K., Narayan, K. M., & Sudharsanan, N. (2024). Predicting control of cardiovascular disease risk factors in South Asia using machine learning. NPJ Digital Medicine, 7(1), 1-10. doi: 10.1038/s41746-024-01353-9.
Sternberg, H., Steinert, J. & Büthe, T. (2024). Compliance in the public versus the private realm: Economic preferences, institutional trust and COVID-19 health behaviors. Health Economics, 33(5), 1055-1119. doi: 10.1002/hec.4807.
Steinert, J., Prince, H., Ezebuihe, J. & Shukla, S. (2023). Violence Against Adolescent Girls During the COVID-19 Pandemic: Quantitative Evidence From Rural and Urban Communities in Maharashtra, India. Journal of Adolescent Health, 73(6), 1010-1018. doi: 10.1016/j.jadohealth.2023.06.006.
Steinert, J., Sternberg, H., Prince, H., Fasolo, B., Galizzi, M., Büthe, T. & Veltri, G. (2022). COVID-19 vaccine hesitancy in eight European countries: Prevalence, determinants, and heterogeneity. Sci Adv, 8(17). doi: 10.1126/sciadv.abm9825.
Steinert, J., Sternberg, H., Veltri, G. & Buethe, T. (2022). How should COVID-19 vaccines be distributed between the Global North and South: a discrete choice experiment in six European countries. eLife. doi: 10.7554/eLife.79819.
Mauer, N., Geldsetzer, P., Manne-Goehler, J., Davies, J.I., Stokes, A.C., McConnell, M., Ali, M.K., Winkler, V. & Sudharsanan, N. (2022). Longitudinal evidence on treatment discontinuation, adherence, and loss of hypertension control in four middle-income countries. Sci Transl Med.; 14(652):eabi9522. doi: 10.1126/scitranslmed.abi9522. Epub 2022 Jul 6. PMID: 35857627.
Sudharsanan, N., Pillai, V.S., Favaretti, C., Jose, J., Jose, S., McConnell, M. & Ali, M.K. (2023). Clinician Adherence to Hypertension Screening and Care Guidelines. JAMA Netw Open.;6(12):e2347164. doi:10.1001/jamanetworkopen.2023.47164
Sudharsanan, N., Wetzel, S., Nachtnebel, M., Loun, C., Phy, M., Kol, H. & Bärnighausen, T. (2022). Know-do gaps for cardiovascular disease care in Cambodia: Evidence on clinician knowledge and delivery of evidence-based prevention actions. PLOS Glob Public Health. ;2(9):e0000862. doi: 10.1371/journal.pgph.0000862.
Stein, D.T., Reitsma, M.B., Geldsetzer, P., Agoudavi, K., Aryal, K.K., Bahendeka, S., Brant, L.C.C., Farzadfar, F., Gurung, M.S., Guwatudde, D., Houehanou, Y.C.N., Malta, D.C., Martins, J.S., Saeedi Moghaddam, S., Mwangi, K.J., Norov, B., Sturua, L., Zhumadilov, Z., Bärnighausen, T., Davies, J.I., Flood, D., Marcus, M.E., Theilmann, M., Vollmer, S., Manne-Goehler, J., Atun, R., Sudharsanan, N. & Verguet, S. (2024). Hypertension care cascades and reducing inequities in cardiovascular disease in low- and middle-income countries. Nat Med.;30(2):414-423. doi: 10.1038/s41591-023-02769-8.
Farbmacher, H., Hartmann, M. & Kögel, H. (2022). Economic Hardship, Sleep, and Self-Rated Health Evidence from the Supplemental Nutrition Assistance Program (SNAP). American Journal of Health Economics; 8(2). doi: 10.1086/717811.
Shaukat, M., Imping, A., Rogge, L., Khalid, F., Ullah, S., Ahmad, F., ... & De Allegri, M. (2024). Un/met: a mixed-methods study on primary healthcare needs of the poorest population in Khyber Pakhtunkhwa province, Pakistan. International Journal for Equity in Health, 23(1), 190. doi: 10.1186/s12939-024-02274-5.
Fischer, T., Frölich, M., & Landmann, A. (2023). Adverse selection in low-income health insurance markets: Evidence from an rct in pakistan. American Economic Journal: Applied Economics, 15(3), 313-340. doi: 10.1257/app.20200639.
Helmsmüller, S., & Landmann, A. (2021). Does free hospitalization insurance change health care consumption of the poor? Short-term evidence from Pakistan. The Geneva Risk and Insurance Review, 1-38. doi: 10.1057/s10713-021-00069-0.
Landmann, A., & Frölich, M. (2015). Can health-insurance help prevent child labor? An impact evaluation from Pakistan. Journal of health economics, 39, 51-59. doi: 10.1016/j.jhealeco.2014.10.003.
Health care management
Sutterer, P., Kolisch, R., & Uzsoy, R. (2022). Valuation of hospital resources: an optimization approach using clearing functions. IISE Transactions on Healthcare Systems Engineering, 12(4), 245-262. doi: 10.1080/24725579.2022.2055236.
Lamprecht, J., Kolisch, R., & Pförringer, D. (2019). The impact of medical documentation assistants on process performance measures in a surgical emergency department. European journal of medical research, 24, 1-8. doi: 10.1186/s40001-019-0390-9.
Gartner, D., Frey, M., & Kolisch, R. (2018). Hospital-wide therapist scheduling and routing: Exact and heuristic methods. IISE Transactions on Healthcare Systems Engineering, 8(4), 268-279. doi: 10.1080/24725579.2018.1530314.
Pförringer, D., Breu, M., Crönlein, M., Kolisch, R., & Kanz, K. G. (2018). Closure simulation for reduction of emergency patient diversion: a discrete agent-based simulation approach to minimizing ambulance diversion. European journal of medical research, 23, 1-8. doi: 10.1186/s40001-018-0330-0.
Fügener, A., Schiffels, S., & Kolisch, R. (2017). Overutilization and underutilization of operating rooms-insights from behavioral health care operations management. Health care management science, 20, 115-128. doi: 10.1007/s10729-015-9343-1.
Gartner, D., Kolisch, R., Neill, D. B., & Padman, R. (2015). Machine learning approaches for early DRG classification and resource allocation. INFORMS Journal on Computing, 27(4), 718-734. doi: 10.1287/ijoc.2015.0655.
Gartner, D., & Kolisch, R. (2014). Scheduling the hospital-wide flow of elective patients. European Journal of Operational Research, 233(3), 689-699. doi: 10.1016/j.ejor.2013.08.026.
Kaiser, F., Schmid, A., & Schlüchtermann, J. (2020). Physician-leaders and hospital performance revisited. Social Science & Medicine, 249, 112831. doi: 10.1016/j.socscimed.2020.112831.
Sturm, H., Schmid, A., Drechsel-Grau, E., & Joos, S. (2022). Derivation of case-mix for intersectoral care in Germany. International Journal of Integrated Care (IJIC), 22. doi: 10.5334/ijic.ICIC22355.
Schmid, A., & Ulrich, V. (2013). Consolidation and concentration in the German hospital market: the two sides of the coin. Health Policy, 109(3), 301-310. doi: 10.1016/j.healthpol.2012.08.012.